Maryland Uniform Credentialing PDF Template
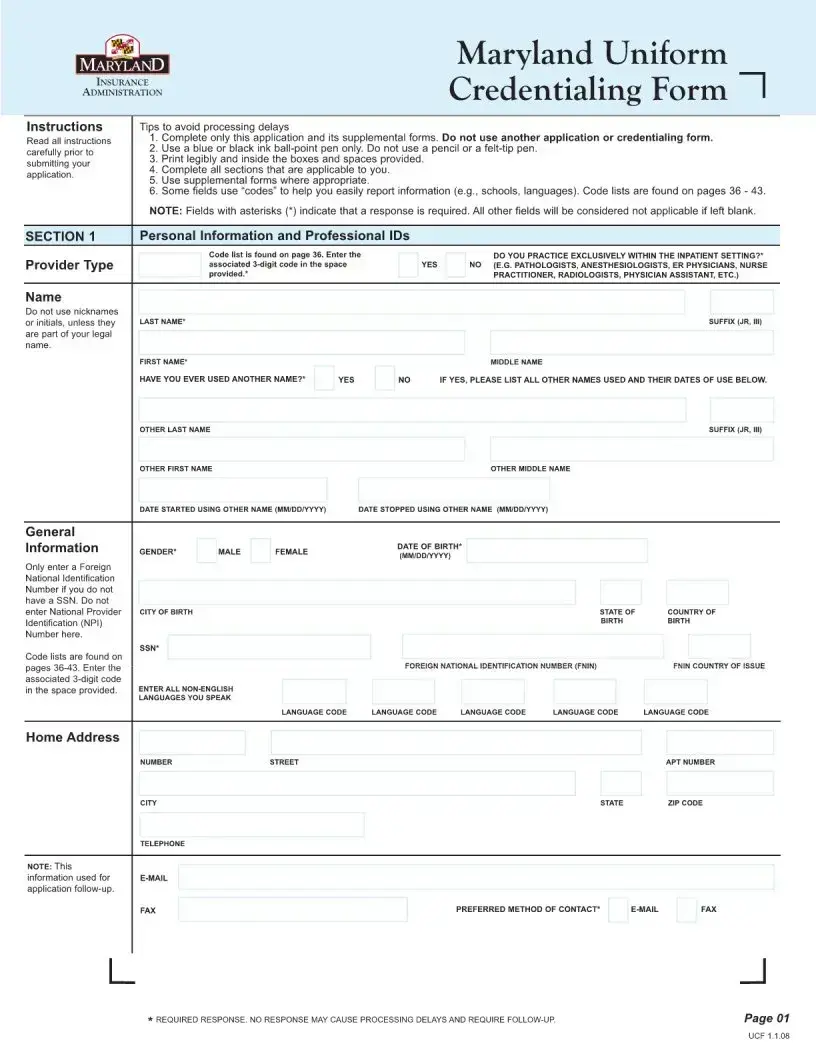
In the world of healthcare, efficiency and standardization are key to providing excellent care and ensuring that professionals are properly verified and credentialed. The Maryland Uniform Credentialing form plays a crucial role in this process, serving as a comprehensive tool that healthcare providers must complete to be credentialed by insurance networks, hospitals, and other healthcare entities in Maryland. This form simplifies the otherwise intricate and time-consuming process of credentialing by consolidating all necessary information into one standardized document. It covers a wide range of information, including personal details, education, training, and work history, as well as any certifications or licenses held by the healthcare provider. Additionally, it helps streamline the verification process, making it easier for providers to demonstrate their qualifications and for entities to review and accept them into their networks. Its implementation reflects Maryland's commitment to improving the healthcare system's efficiency, ensuring that providers can focus more on patient care and less on administrative tasks.
Maryland Uniform Credentialing Sample
File Breakdown
| Fact Name | Description |
|---|---|
| Purpose | The Maryland Uniform Credentialing Form is designed to simplify the process of credentialing for healthcare providers, allowing them to submit their qualifications to multiple health plans and healthcare systems via a single standardized form. |
| Governing Law | The form is governed by Maryland state law, specifically the provisions related to healthcare provider credentialing processes. This ensures a uniform approach to credentialing across the state. |
| Who Uses It | Healthcare providers, including doctors, nurses, and other medical professionals in Maryland, use this form when applying for privileges or participation in health plans. |
| Where to Submit | Completed forms are typically submitted to health plans, hospitals, or other healthcare organizations that require provider credentialing as part of their network participation criteria. |
| Benefits | It streamlines the credentialing process, reduces paperwork, and saves time for both providers and healthcare entities. This standardized approach also helps reduce errors and inconsistencies in provider information. |
| Requirements | Providers must fill out the form with accurate and up-to-date information about their professional qualifications, work history, malpractice insurance, and any certifications or specialties. |
| Validity Period | While the form itself does not expire, credentialing is not permanent and must be periodically renewed according to the specific policies of the healthcare entity or plan. |
| Where to Find | The form can typically be found on the websites of Maryland state health departments, professional licensing boards, or directly from health plans and healthcare institutions requiring the credentialing. |
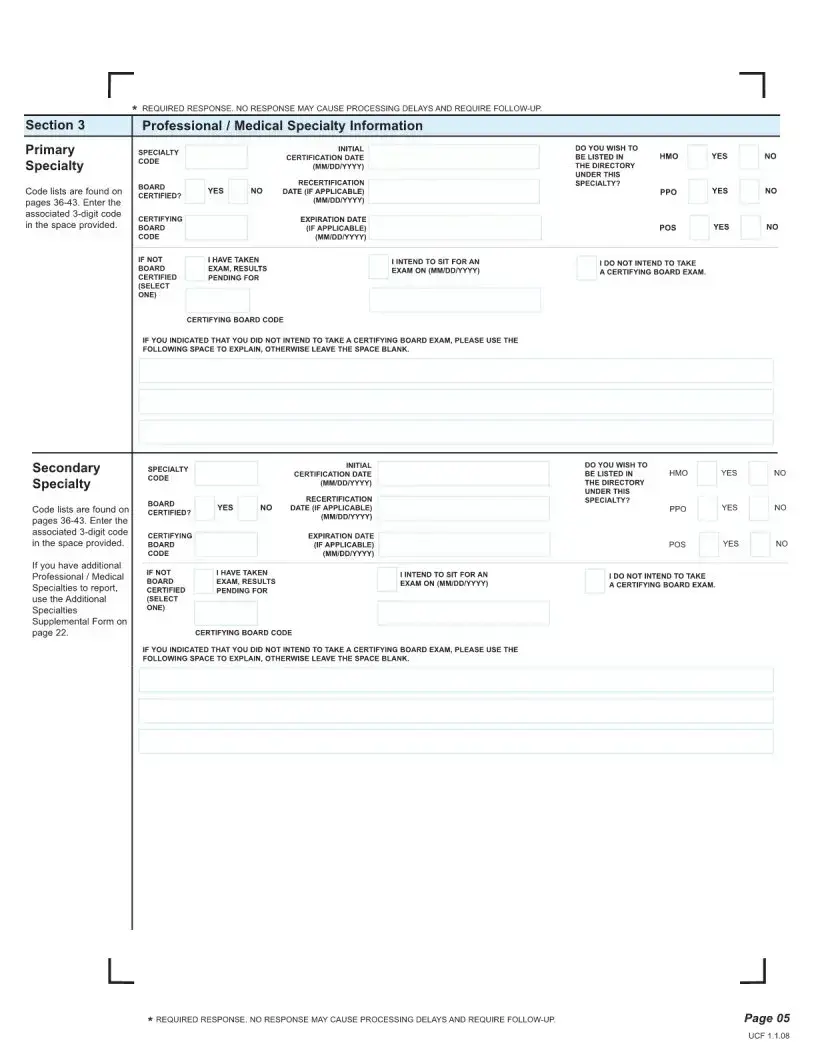
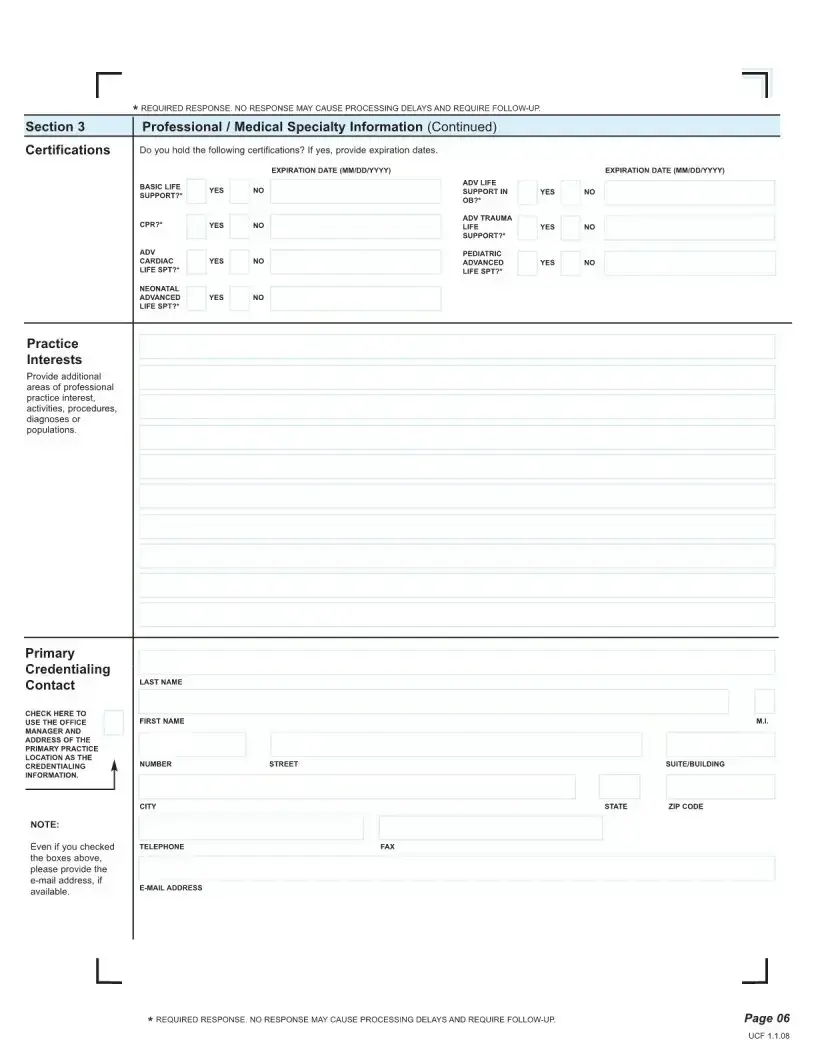
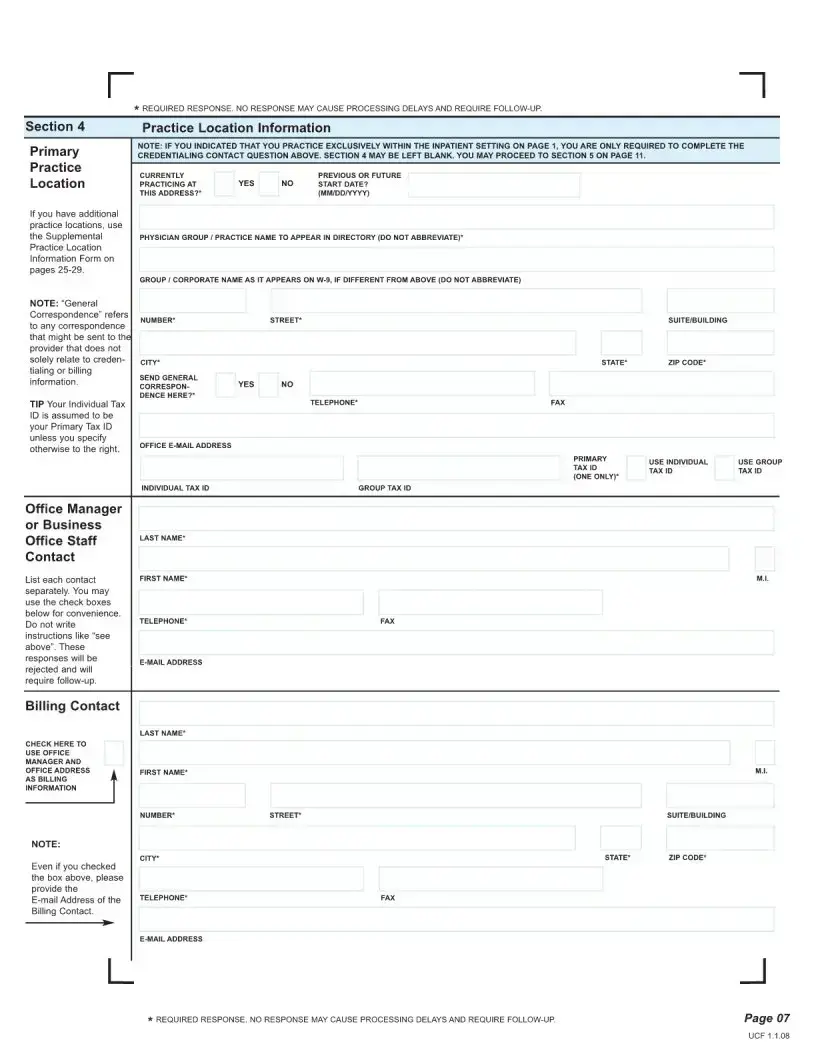
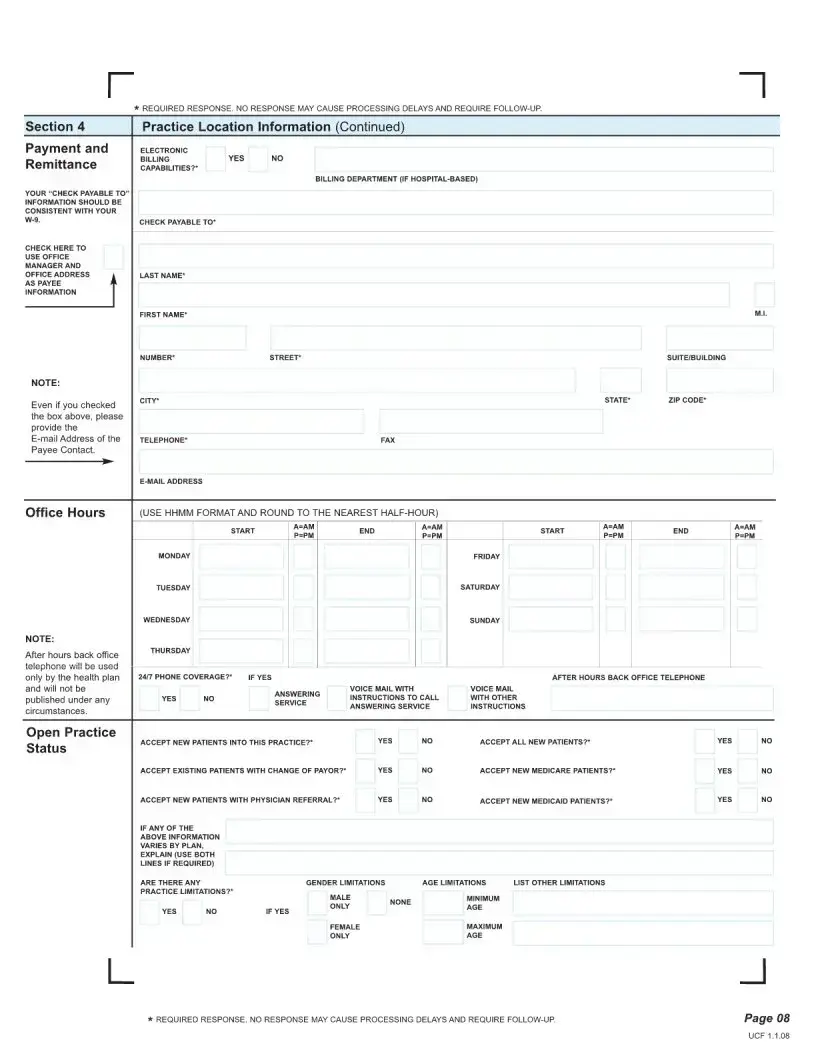
Steps to Filling Out Maryland Uniform Credentialing
After completing the Maryland Uniform Credentialing form, it will be processed to ensure all healthcare professionals seeking to provide services in Maryland are appropriately verified and registered. This step is crucial for maintaining the integrity and quality of healthcare services in the state. Once submitted, the form will be reviewed for completeness and accuracy. It's important to provide all requested information correctly to avoid delays.
- Begin by entering your personal information, including your full name, social security number, and date of birth.
- Specify your contact information, such as your email address, phone number, and mailing address.
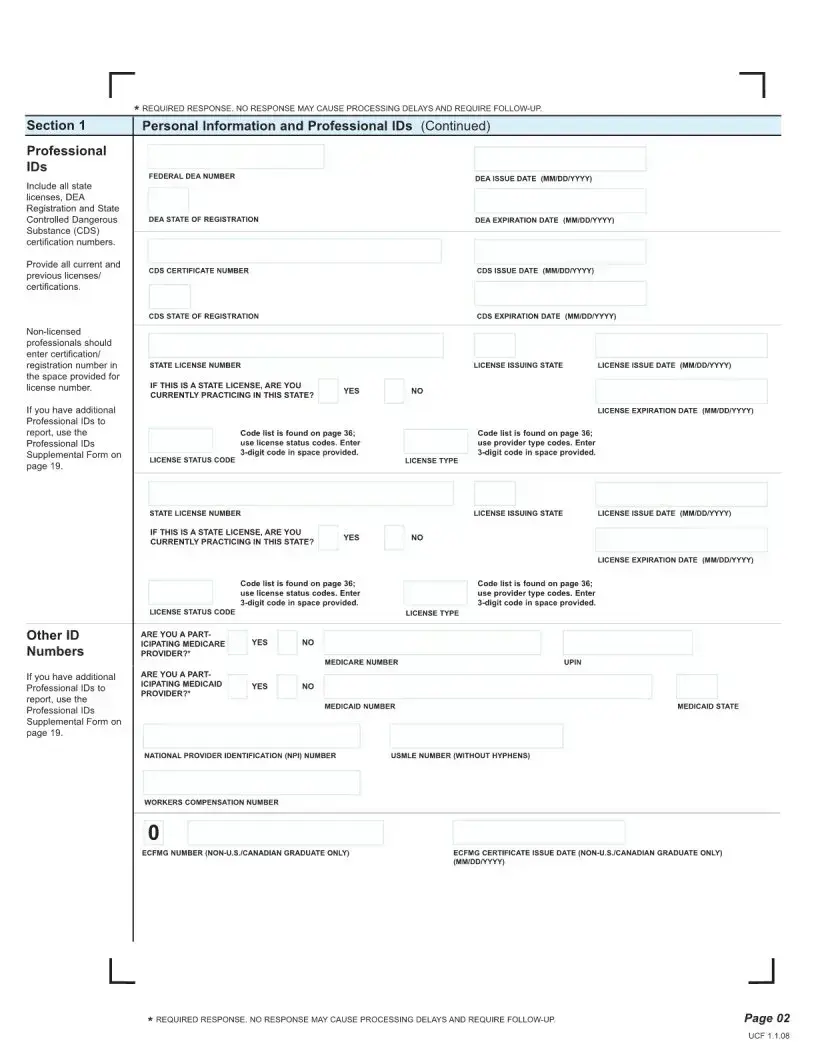
- Indicate your professional information, including your professional title, area of specialty, and Maryland licensure number.
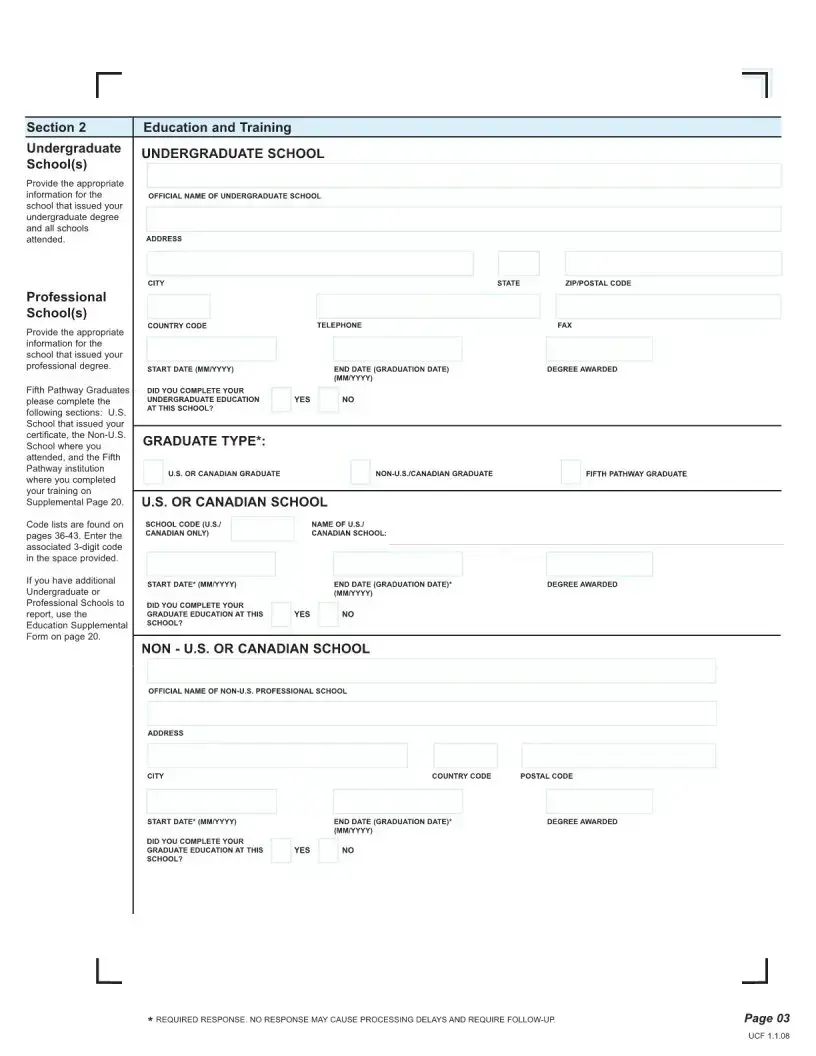
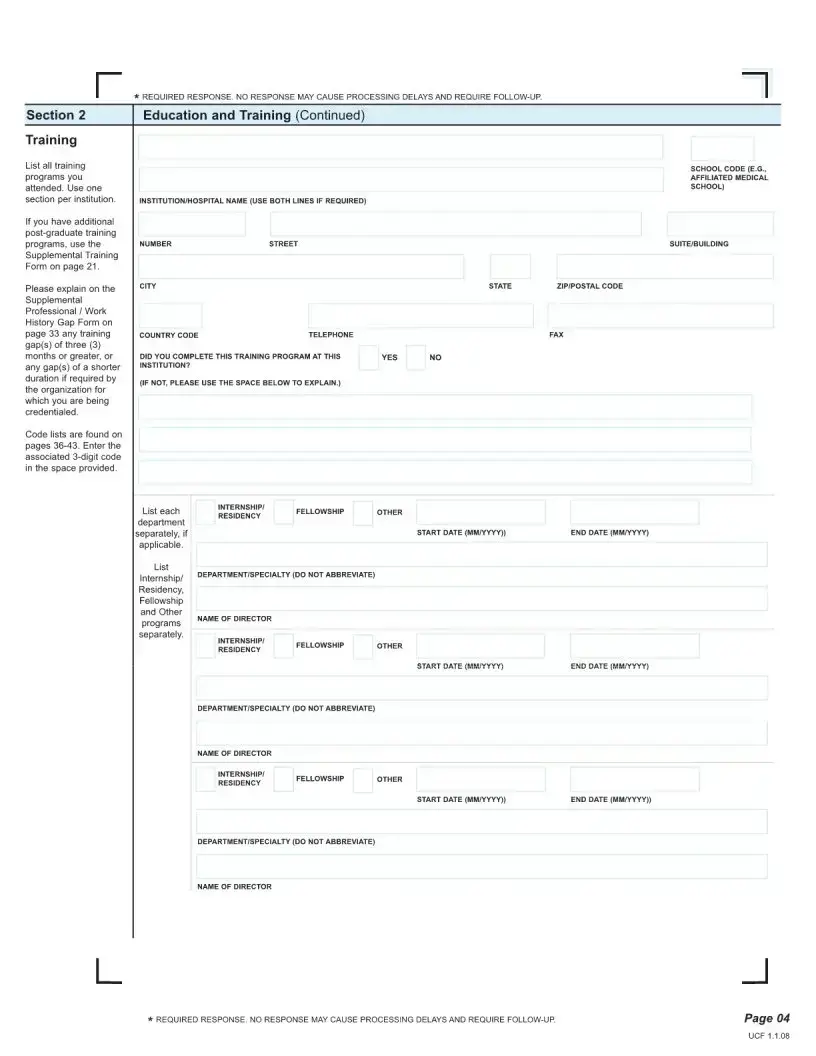
- List all professional education and training, including institutions attended, degrees earned, and dates of attendance.
- Detail your work history for the past five years, including employer names, positions held, and dates of employment.
- Provide information about any professional affiliations, such as memberships in medical associations or societies.
- Answer questions related to your professional conduct, including any disciplinary actions, malpractice claims, or criminal convictions.
- Attach supporting documentation as required, including copies of your professional licenses, certificates, and any other credentials.
- Review your answers carefully for accuracy and completeness before proceeding to the next step.
- Sign and date the form to certify that the information provided is true and complete. Electronic signatures may be accepted if the form is submitted online.
- Submit the form and any additional required documentation as directed. This may include mailing it to a specific address or uploading it through an online portal.
Once the form has been submitted, it's important to keep a copy for your records. You may be contacted for additional information or to clarify the details provided. Processing times can vary, so it's advisable to submit the form well in advance of when credentialing or recredentialing is needed.
More About Maryland Uniform Credentialing
What is the Maryland Uniform Credentialing Form?
The Maryland Uniform Credentialing Form is a standardized document used by healthcare providers in Maryland to apply for credentials or privileges at healthcare organizations, such as hospitals and health insurance networks. The form streamlines the process by consolidating the required information into a single document, making it easier for both providers and organizations to handle credentialing applications.
Who needs to complete the Maryland Uniform Credentialing Form?
Healthcare providers who wish to join a hospital, clinic, or health plan network in Maryland should complete the Maryland Uniform Credentialing Form. This includes doctors, nurses, therapists, and other healthcare practitioners seeking to offer services through these institutions. Completing and submitting this form is a crucial step in the credentialing process, which allows a healthcare provider to practice within a specific organization.
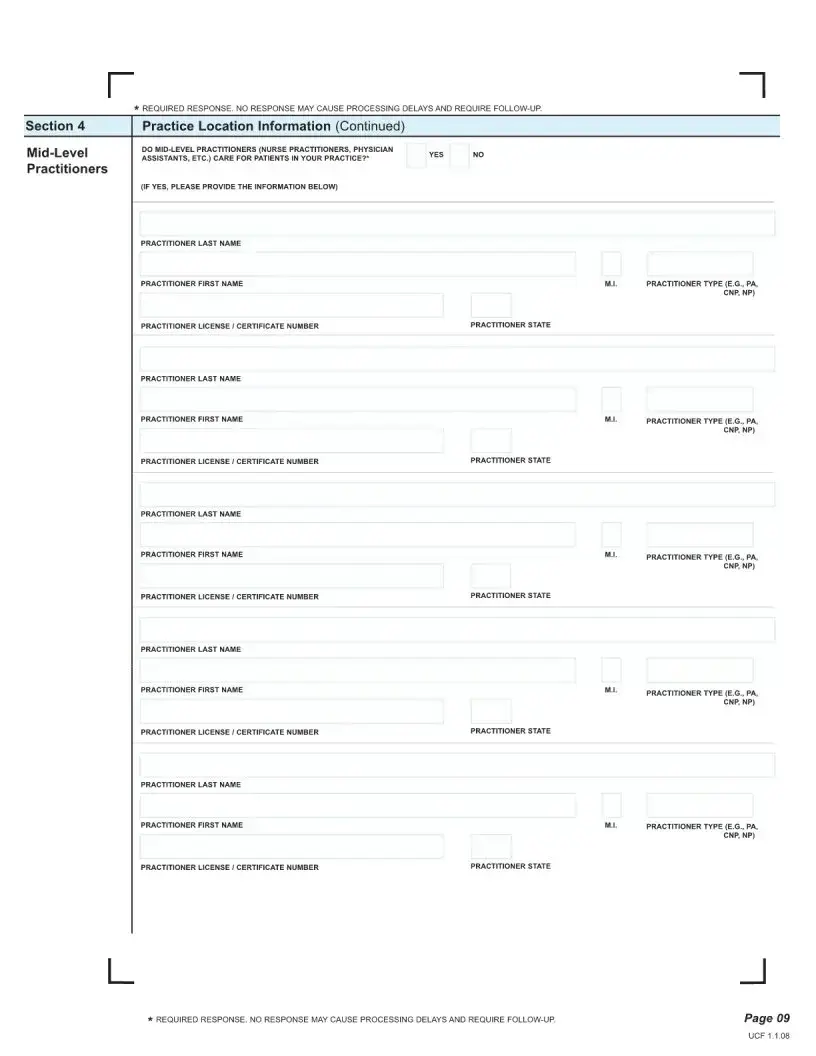
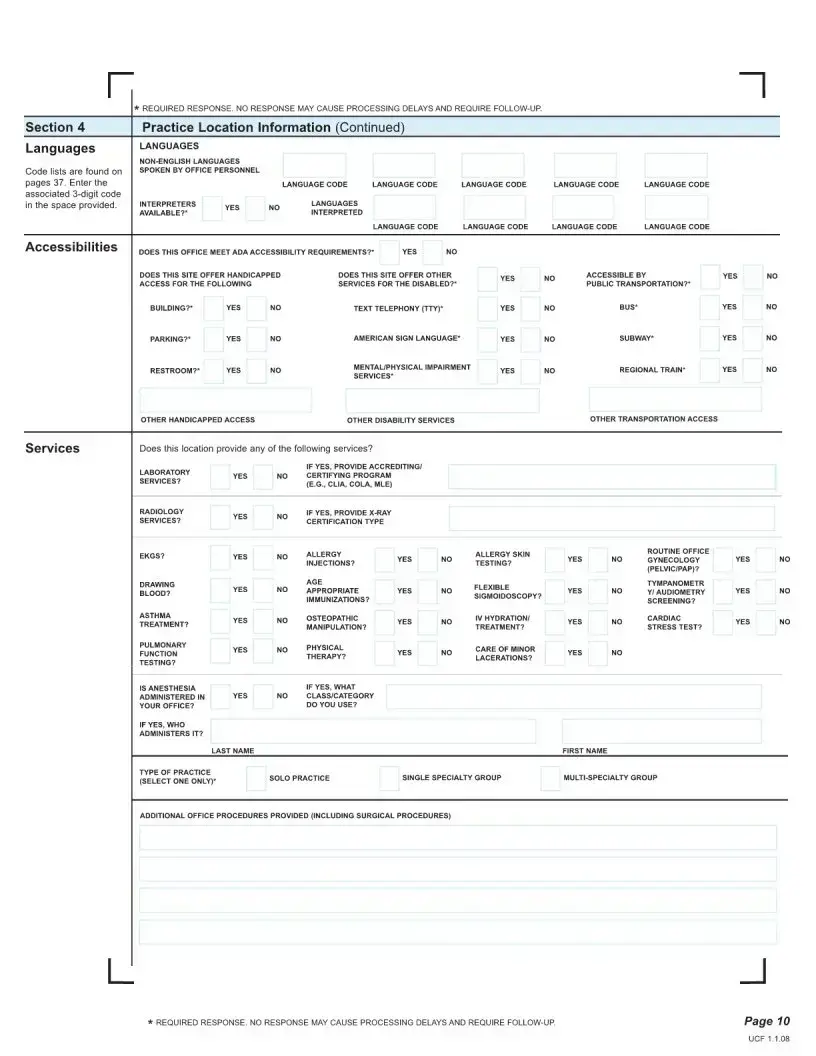
What information is required on the Maryland Uniform Credentialing Form?
The form requests a variety of information necessary for the credentialing process, including:
- Personal and professional information (such as name, contact details, and Social Security number)
- Educational background (including schools and dates of attendance)
- Work history (listing all healthcare positions)
- Professional licenses and certifications (type, number, and expiration date)
- Professional liability insurance coverage details
- Information on any disciplinary actions or malpractice claims
It is crucial to provide accurate and complete information to avoid delays in the credentialing process.
How can a provider submit the Maryland Uniform Credentialing Form?
The completed Maryland Uniform Credentialing Form can be submitted in one of two ways:
- Electronically, via the email or web portal specified by the healthcare organization or insurance network. This is often the preferred method for its ease and efficiency.
- By mail, if the receiving organization allows for it, to the address provided by them. It's important to check with the specific organization for any special mailing instructions.
Providers should ensure that they receive a confirmation of receipt to verify that their application is being processed.
Is there a deadline for submitting the Maryland Uniform Credentialing Form?
The deadline for submitting the Maryland Uniform Credentialing Form varies by healthcare organization and insurance network. It is advisable to submit the form well in advance of when you wish to start providing services or at the onset of the renewal process for existing credentials. Providers should check directly with the organization to which they are applying for specific deadlines.
What happens after the Maryland Uniform Credentialing Form is submitted?
After submission, the credentialing department of the receiving organization will review the form for completeness and verify the provided information. This process may include checking the provider's educational background, license validity, work history, and any malpractice history. Providers may be asked to furnish additional information or clarification during this time. Once the review is complete, the organization will notify the provider of their credentialing status. This process can take several weeks to months, depending on the organization's procedures and the completeness of the application.
Common mistakes
-
Failing to double-check for accuracy. When individuals rush through filling out the form, they may overlook spelling errors, especially in their personal information or credentials. This could delay the credentialing process or cause unnecessary complications.
-
Skipping sections that appear irrelevant. Sometimes, sections that seem not to apply directly may still require a response, such as "Not Applicable" or "N/A." Leaving these sections blank could be interpreted as an oversight or incomplete form.
-
Omitting necessary documents. The form often requires supplementary documentation, like proof of qualifications or certifications. Forgetting to attach these documents can result in an incomplete application.
-
Not using a pen with black ink. While this may seem trivial, filling out the form in any other color can cause issues, especially if the document needs to be scanned or copied, as other colors might not reproduce clearly.
-
Assuming experience will compensate for missing information. Sometimes, individuals might think that their extensive experience can make up for not fully completing the form or providing detailed responses. However, every section of the form is required for a thorough evaluation.
-
Ignoring the signature and date section. This is perhaps one of the most crucial oversights. An unsigned or undated form is often considered invalid and will not be processed until this mistake is rectified.
When completing the Maryland Uniform Credentialing Form, paying attention to detail and carefully reviewing each section before submitting it is essential. This ensures the process moves forward smoothly and without delay.
Avoiding common mistakes like these not only streamlines the credentialing process but also reflects well on the applicant's professionalism and attention to detail.
Documents used along the form
When healthcare providers in Maryland apply for hospital privileges or participate with insurance companies, they often use the Maryland Uniform Credentialing form as part of the application process. This form is integral in verifying the credentials of healthcare providers. Alongside this essential form, several other documents are commonly submitted to support the application process. The following list includes some of these important documents, each with a description of its role in complementing the Maryland Uniform Credentialing form.
- Curriculum Vitae (CV): This comprehensive document outlines the applicant's education, work history, professional achievements, and other relevant experience. It provides a detailed overview of the applicant’s qualifications and career progression.
- Professional Liability Insurance Certificate: This certificate serves as proof that the applicant has the necessary malpractice insurance. Insurance coverage is a crucial requirement, protecting both the healthcare provider and the patients.
- Board Certification Documents: These documents verify that the applicant has achieved certification in their medical specialty. Board certification demonstrates a level of professional expertise and commitment to ongoing education.
- Drug Enforcement Administration (DEA) Certificate: For healthcare providers who prescribe medication, this certificate is mandatory. It indicates that the provider is authorized by the federal government to prescribe medications.
- State License: An up-to-date state license is required to practice medicine within Maryland. This document confirms that the healthcare provider is legally permitted to provide medical services in the state.
- Continuing Education Certificates: These certificates show that the healthcare provider has participated in ongoing education efforts relevant to their specialty, demonstrating their commitment to maintaining competence in their field.
- References or Letters of Recommendation: Letters from colleagues or supervisors that speak to the healthcare provider's skills, ethics, and professionalism offer additional insights into their suitability for practice or credentialing.
Together, these documents play a crucial role in the credentialing process, providing a more complete picture of the healthcare provider's qualifications, experience, and professional standing. They support the information provided in the Maryland Uniform Credentialing form, ensuring a thorough evaluation of the provider’s credentials. This detailed approach helps maintain high standards of care and professionalism within Maryland's healthcare system.
Similar forms
The Maryland Uniform Credentialing form is similar to several other documents used within the healthcare industry for the purpose of credentialing and verifying the qualifications of healthcare providers. Each document, while serving a similar purpose, has unique features that cater to specific requirements of various organizations or regulatory bodies.
The National Practitioner Data Bank (NPDB) Continuous Query Authorization Form: This form is akin to the Maryland Uniform Credentialing form in its function to uphold the standards of healthcare providers' credentials. Both forms collect detailed information on a provider's qualifications, history of professional conduct, and disciplinary actions. However, the NPDB Continuous Query Authorization Form uniquely allows healthcare entities to receive ongoing notifications about any changes to a practitioner's record, ensuring continuous monitoring of providers' eligibility to provide care.
The Healthcare Provider Taxonomy Code Request Form: Like the Maryland Uniform Credentialing form, this document is crucial for correctly identifying healthcare providers' roles and specialties. Both forms include sections where providers must list their qualifications, certifications, and areas of specialty. The Taxonomy Code Request form specifically requires providers to obtain and use unique identifiers which facilitate billing and administrative tasks, distinguishing it by its focus on streamlining financial and administrative operations within healthcare organizations.
Council for Affordable Quality Healthcare (CAQH) ProView Profile: The CAQH ProView platform serves a parallel purpose to the Maryland Uniform Credentialing form by collecting comprehensive profiles of healthcare providers for credentialing. Both require detailed personal and professional information, including education, work history, and board certifications. The CAQH ProView stands out by offering a centralized digital repository that providers can update periodically, which healthcare organizations across the country can access, promoting efficiency and reducing the need for multiple submissions of the same information.
Dos and Don'ts
Filling out the Maryland Uniform Credentialing form is an important step for healthcare providers wishing to facilitate their credentialing process. When completing this form, accuracy and attention to detail are paramount. Below are key dos and don'ts to consider during this essential process.
Do:
- Read through the entire form before beginning to understand all the required information and how it should be presented.
- Ensure that all information provided is accurate and up-to-date, particularly personal details, work history, and educational background.
- Use a black or blue pen if the form is filled out by hand, as these colors are typically required for official documents and ensure legibility.
- Include all necessary attachments, such as copies of licenses, certifications, and other pertinent documents that support your application.
- Double-check for any errors or omissions before submission, as even minor mistakes can delay the credentialing process.
- Contact the responsible department or agency directly if you have any questions or need clarification on specific sections of the form.
Don't:
- Leave any sections incomplete, unless specifically instructed to do so. If a section does not apply, write “N/A” to indicate this.
- Submit the form without first making a copy for your records. It's crucial to have a backup in case the original is lost or you need to refer back to it.
- Rush through the form, as this can lead to mistakes. Take your time to fill it out carefully and thoughtfully.
- Use correction fluid or tape. Instead, if you make a mistake, start over with a new form to maintain a professional appearance.
- Overlook the deadline for submission. Late applications can result in delays or may not be accepted at all.
- Forget to sign and date the form. An unsigned or undated form is considered incomplete and will not be processed.
By following these guidelines, healthcare providers can smoothly navigate the Maryland Uniform Credentialing form process, ensuring a more efficient and successful credentialing experience.
Misconceptions
When it comes to understanding the Maryland Uniform Credentialing Form, several misconceptions can arise. These misconceptions can cause confusion and delay in the credentialing process. Below, we'll address ten common misunderstandings and clarify the facts to help navigate the use of this form more effectively.
It’s only for doctors: The Maryland Uniform Credentialing Form isn't just for doctors. It’s also for other healthcare providers such as dentists, nurses, and therapists who need to be credentialed with insurance companies, hospitals, and other healthcare entities.
Credentialing is instant: Filling out the form is a step in the credentialing process, but it doesn't mean immediate approval. The process involves verification of information and can take several weeks or even months to complete.
One time is enough: Credentialing isn’t a one-and-done deal. Providers need to periodically re-credential, typically every two to three years, to ensure their information is current and they remain in compliance with evolving standards.
The form is universal: While the form is widely accepted in Maryland, it may not fulfill all credentialing requirements for every organization or insurer. Some may have additional forms or specific requirements.
Personal information isn't necessary: The form requires personal information, including social security numbers and educational background. This data is essential for identity verification and background checks.
Handwritten forms are acceptable: To prevent errors and ensure legibility, the preference is often for the form to be typed. However, if handwriting is necessary, it must be legible. Always check with the requesting organization.
It’s the only step for hospital privileges: Securing hospital privileges involves more than just the Maryland Uniform Credentialing Form. Hospitals typically conduct a thorough review, including interviews and assessments of clinical competence.
Errors on the form aren’t a big deal: Even minor errors or omissions can delay the credentialing process. It’s crucial to review the form carefully before submission to ensure all information is accurate and complete.
Digital signatures are always accepted: While many organizations accept digital signatures, some may require a wet signature. It’s important to verify the signature requirements of the organization to which you're submitting the form.
It doesn’t need to be updated if nothing has changed: Even if there have been no changes to your status, you may still be required to resubmit or update the form periodically to confirm your information remains accurate.
By understanding these common misconceptions about the Maryland Uniform Credentialing Form, healthcare providers can navigate the credentialing process more smoothly and avoid unnecessary setbacks. Remember, when in doubt, it's always best to communicate directly with the specific organization or insurance company to confirm their requirements and processes.
Key takeaways
The Maryland Uniform Credentialing form plays a critical role for healthcare providers in Maryland, streamlining the process of applying for privileges or affiliations with various health plans, hospitals, and other health care entities. Understanding how to fill out and use this form properly can save time and ensure a smoother credentialing process. Here are five key takeaways:
- Accuracy is key: When filling out the Maryland Uniform Credentialing form, it's crucial to provide accurate and up-to-date information. Any discrepancies or errors can delay the credentialing process, potentially affecting your ability to provide services.
- Complete every section: Do not leave any section of the form blank unless it's explicitly stated as optional. Incomplete forms may be returned to you, causing delays. If a section does not apply to you, indicate with “N/A” (not applicable).
- Required documents: The form will usually ask for supplementary documents to support the information you've provided. These may include copies of your professional license, proof of malpractice insurance, and past work history. Ensure all documents are current and clearly legible.
- Keep personal information updated: If any of your personal information changes after you've submitted the form (such as address, contact information, or professional licenses), you should notify all relevant parties promptly. This helps maintain the integrity of your credentialing status.
- Know the renewal process: Credentialing is not a one-time process. Be aware of the expiration dates of your credentials and start the renewal process well in advance. The Maryland Uniform Credentialing form may be required again for this process, so staying organized and keeping copies of previously submitted forms can be helpful.
Properly utilizing the Maryland Uniform Credentialing form is a fundamental step for healthcare providers seeking to establish or expand their practice in Maryland. Being diligent, thorough, and proactive in filling out and submitting this form can significantly impact the efficiency of your credentialing process.
Common PDF Templates
State of Maryland Employee Health Insurance Premiums - This form helps to streamline the process of obtaining vision coverage, reducing administrative delays and confusion.
What's the First Thing to Do When Starting a Lab? - A vital tool for laboratories in Maryland to maintain accurate, up-to-date licensing records.